Patient engagement and care collaboration:
Another wasted opportunity?
Updated 2019-09-25 4:00 pm
In our last post, we looked at the recently released White House report “The State of Homelessness in America.” Among other things, the report notes that under previous administrations, housing programs, most of which follow the Housing First model, have not required housing beneficiaries to participate in supportive service programs, such as those for addiction, mental illness, chronic physical health, employment, education or offender reentry. The report makes the case that the failure of past housing administrations to require such participation is one of the reasons for the low or at least mixed rates of success by these programs and therefore contributes to higher rates of homelessness.
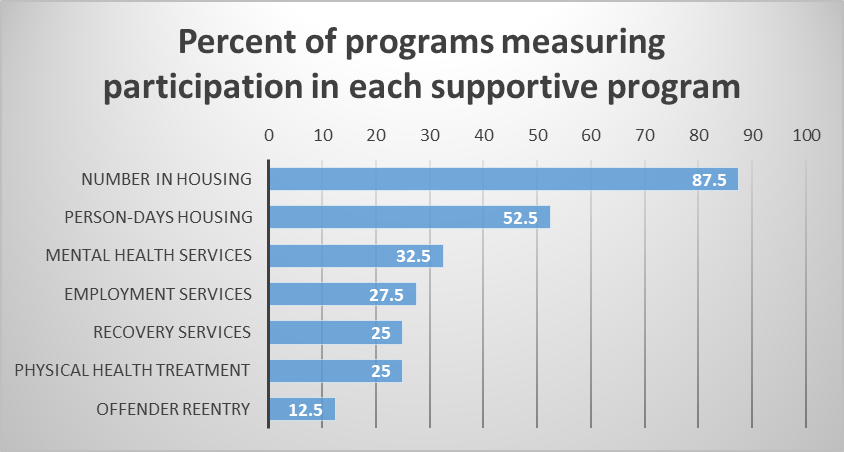
The largest single program designed to help people experiencing homelessness is the Permanent Supportive Housing (PSH) program. In April, we conducted a Survey of Evidence-based Practices and Technology Use in PSH Programs to learn more about how closely housing programs align their services with other supportive service programs. Survey results showed that while the Housing First evidence-based practice advises that housing providers should promote participation in supportive service programs, fewer than 1/3 of housing providers measure participation in supportive service programs. Similarly, only about 27% of programs measure health service utilization and only 18% measure cost, both measures of health outcomes.
Our survey did not attempt to evaluate how effective these programs are at reducing homelessness or improving health outcomes. Nonetheless, our study results are consistent with the report’s assertion that housing programs have not traditionally been closely aligned to supportive services. This raises the question whether greater emphasis on engagement and collaboration between housing providers and other supportive service providers could have a significant positive impact on homelessness, improving health outcomes and lowering cost. Whether a program with a hard requirement for participation will be more effective than one with stronger incentives but not a hard requirement is not clear from past research. Therefore, the Administration’s proposed reform requiring such participation is worth consideration and, possibly, study.
Most Federal funding for housing comes through the Department of Housing and Urban Development (HUD). The largest funding program is the Continuums of Care (CoC) program that, for 2019, has a budget of about $2.3 billion. The report notes “the 2019 Notice of Funding Availability (NOFA) [for the CoC program] allows communities flexibility to impose service participation requirements for participants after they have been stabilized in housing. This reform will allow for greater local flexibility and innovation to drive successful outcomes for vulnerable homeless individuals.”
That sounds reasonable as a policy recommendation, but, as the cliché goes, the devil is in the details. We wondered what, exactly, is in the 2019 funding guidance for CoC? Specifically, are these new policy priorities reflected in the scoring model used to award money?
The only reference to requirements for participation in supportive services is in a section titled “Providing Flexibility for Housing First with Service Participation Requirements,” which concludes “…so this NOFA also provides communities and programs with flexibility, without penalty, to use service participation requirements after people have been stabilized in housing.”
Next we looked to the scoring model for funding applications. The CoC program uses a 200 point scale with points assigned for a wide range of criteria. We found no criteria where points would be influenced by requiring participation in supportive services. These are the critical measures that the CoCs and housing agencies use to establish their program priorities, so their absence in the scoring model suggests these policies will not be high priorities for either CoCs or housing agencies.
While the idea of providing more focus on engaging beneficiaries in supporting services makes intuitive sense, we are not aware of evidence that supports a hard requirement for participation—but we’d love to study it, along with other methods of increasing participation.
Grant applications for 2019 are due September 30. It will be interesting to see if the permission granted in the NOFA, combined with policy guidance from officials, will result in new programs that require participation in supportive services. In the absence of grant awards under the new policy, we have to conclude that with only a modest reference to allowing programs to require participation, and providing no new guidance in the scoring section to encourage CoCs or housing providers to reform Housing First practices as suggested, this recommendation by itself, will have little effect, and may indeed be a wasted opportunity.
But that isn’t the whole story. In another post, we’ll talk about the more significant, albeit nuanced, undercurrents that are moving us towards a truly integrated continuum of care.
Hint: Follow the money.


This is the first time I’ve read this publication and I really enjoyed it. This is an area that deserves robust debate and dialogue. However, as a recipient of CoC PSH funds I can attest that it has been clearly stated by HUD and others, such as the state of California and our local CoC, that service participation requirements have previously been strictly prohibited under the Housing First model. For example, during renewal applications, we actually turn in leasing documents that must clearly state that services are not a requirement for initial or continued assistance. Just thought I’d make that point. Thanks!
Thank you Mr. Walters. I have updated the post to reflect your valuable contribution.