proVizor Telehealth Community Project
advances recommendations of NQF and CQMC
In a recent post, we discussed some of the current legislative actions and executive orders that promote innovation in telehealth technology and funding to improve outcomes and lower cost. In this post, we comment on industry initiatives to support the inevitable evolution towards telehealth and what White Pine is doing to advance those recommendations.
Defining telehealth
Telehealth refers to the set of online and mobile tools that extend evidence-based practice (EBP) beyond the walls and hours of the clinic or organization. As used here, telehealth refers to “asynchronous” interactions, meaning that the consumer interacts with the application without a clinician or staff person participating in the interaction at the same time. Telehealth contrasts with telemedicine where the technology facilitates real-time, “synchronous” interactions between consumers and clinicians or staff.
Telehealth opportunities
Telehealth offers the potential to improve outcomes and lower cost across the health and social continuum. Opportunities exist both within the EBP for a particular health concern or interest, what we call a “Care Unit,” and between Care Units, recognizing the inherent interaction between and among health and social conditions. One of the most glaring opportunities is at the intersection of physical health, behavioral health and Social Determinants of Health (SDOH) which have developed into separate silos with little interoperability or coordination between them. Within SDOH, opportunities for telehealth include permanent supportive housing programs for people experiencing homelessness and offender reentry for people recently released from incarceration.
As we consider regulatory and industry initiatives, we’re looking not only at solutions that translate EBP into technology-enabled applications but also for solutions that break down the barriers between physical health, behavioral health and SDOH. In that spirit, we are pleased to see several recent initiatives from the industry, such as those advanced by the National Quality Forum (NQF).
NQF SDOH Action Brief
In July, the NQF published an action brief issued on behalf of “The Social Determinants of Health Data Integration Action Team,” a group of about 50 industry leaders, that sets forth 8 priority challenges and 3 recommendations to improve the integration of SDOH into the health care continuum. The action brief brings focus to things that, frankly, are pretty obvious: that integration of SDOH into the healthcare continuum is hindered by a lack of standards and definitional issues between sectors, inadequate capacity, concerns about the accuracy of data and insufficient payment mechanisms. The recommendations are also obvious: standardize and share data, demonstrate collaboration across sectors and evaluate effectiveness. (The action brief is truly brief, coming in at 4 pages. You can download it here.)
National Call to Action
Then, on October 24, the NQF, along with the Aetna Foundation, published a more detailed “National Call to Address Social Determinants of Health through Quality and Payment Innovation” that[D1] calls on payers, clinicians, community-based organizations, hospitals and health systems and others to:
- Align policies, funding and reimbursement;
- Develop key sets of measures;
- Execute the recommendations of the earlier Action Brief;
- Provide funding to test, collect data, assess and measure, and;
- Incentivize and reward healthcare organizations at multiple levels.
These are “mom and apple pie” recommendations—who’s gonna argue with these? Nonetheless, that they expressed as a national call to action by organizations such as the NQF and the Aetna Foundation is significant.
CQMC common measures
Finally, yesterday, November 14, the NQF, acting on behalf of the Care Quality Measures Collaborative (CQMC), published a draft paper titled “Approaches to Core Set Prioritization” and opened it for a brief comment period. (The comment period closes on November 22 at 6:00 pm Eastern.) The paper is a discussion of the need and recommendations for how to approach a common set of metrics that will simplify and inform all stakeholders across the continuum of care, in alignment with the second recommendation from the National Call mentioned above.
But here’s the interesting thing: Nowhere in the CQMC draft document are SDOH measures even mentioned. This is not too surprising as we observe that such significant changes to health and social care models are about as easy to accomplish as turning the Titanic before hitting an iceberg. As the paper notes, the CQMC is building from its initial set of 8 ambulatory domains and invites recommendations for others. Thus, despite the absence of SDOH measures in this draft, we are pleased to see the progress broadly and the leadership of organizations like the NQF. We will most certainly submit a comment with our recommendation.
proVizor advances the recommendations
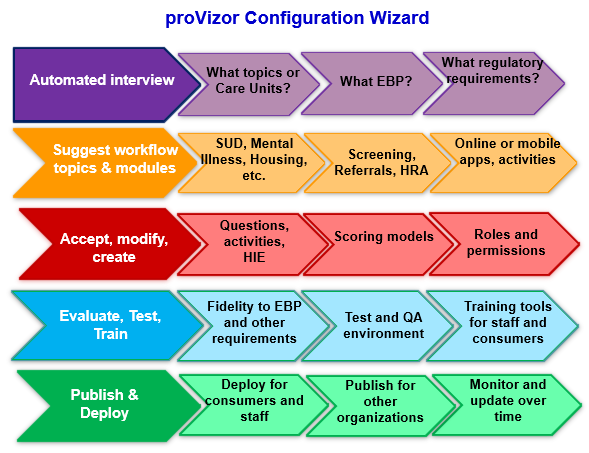
But advancing the vision and defining approaches isn’t enough. As each of these initiatives makes clear, we need action. At White Pine, we’ve been waiting for this moment for years. It is obvious both that SDOH must be better integrated into the continuum of care and that technology is key to that integration. Implicit in each of these reports and policy initiatives is the need not only for the technology itself but for a new, better, more cost effective way to implement technology in an evolving environment. We’re doing our part. Our earlier work demonstrated impressive improvements in outcomes and operating efficiency for people in recovery. Now our patent-pending proVizor Configuration Wizard will allow workflow administrators of all experience levels to easily and efficiently create, evaluate, train for and maintain electronic workflows that reliably meet a particular evidence-based practice, standard or regulatory requirement, and/or provide reliable question or activity response data (e.g., reliable user behavior and feedback data) without the need to engage outside consultants or programmers, thus reducing the time and cost of creating and maintaining an effective electronic workflow. This includes the ability to test and support evolving metrics across the continuum of care.
proVizor Telehealth Community Project
Starting this month, we are supporting these telehealth initiatives through the proVizor Telehealth Community Project, a three year project consisting of technologists, academics, health and social care providers and consumers to identify business requirements, design functional requirements, test, deploy and evaluate innovative solutions in patient engagement and care coordination. Starting with our solid foundation of experience and success, this is the necessary next step—to empower practitioners to design, modify, deploy and evaluate their own EBP workflows across the continuum of care.
It is clear that from a policy perspective and from an industry leadership perspective, now is the time take action. The proVizor Telehealth Community Project is the perfect opportunity to make a difference.
For the initial phase, we’re looking for health and social care providers in the following areas to join the community:
- Substance Use Disorder
- Mental Health
- Permanent Supportive Housing
- Offender Reentry
- Physical health (management of chronic conditions)
To learn more, please visit the proVizor Telehealth Community Project.

