The Age of Telehealth is at Hand--Maybe!!
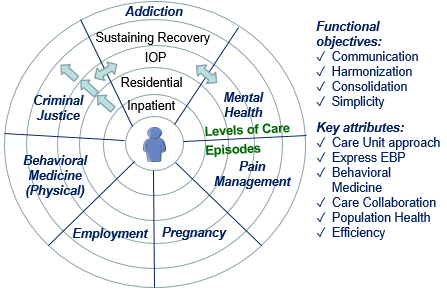
The proVizor Care Collaboration Wheel
You can be excused if you’ve missed this. It hasn’t been the top line, but inside recent policy announcements, including legislation, regulatory pronouncements and executive orders is clear policy guidance leading to a period of innovation in telehealth that may have the potential to revolutionize health and social care by bridging the gaps that have previously isolated physical health, behavioral health and social care through technology-enabled workflows that simplify patient engagement and care collaboration.
At the core are two common sense changes that are ubiquitous in the rest of our lives but have not yet been adopted in health or social care:
- Break down the silos between physical health, behavioral health and social supports to create one, truly integrated continuum of care, and;
- The adoption of low cost, easy to use telehealth workflows that extend evidence-based practice beyond the walls and hours of the clinic or facility.
The result could be a significant improvement in health, lower cost, and an increase in both provider and consumer satisfaction. It’s hard to think of a more dramatic or important advance in the health and social welfare of the nation.
I have been wrong before. Wrong. Wrong. Wrong.
I confess. This isn’t the first time I’ve thought we were on the cusp of such an important transformation. I was wrong with the Affordable Care Act, the Excellence in Mental Health Act, MACRA and, it seems to me, a dozen other initiatives that sounded like they created a compelling incentive for telehealth innovation. With the benefit of 20/20 hindsight, it is easy to see that whatever incentive may have been intended, the larger history of pointless and ever changing regulations and requirements, combined with a yo-yo like revenue strategy, has led providers to do the least they could to meet new requirements unless it was absolutely certain the guidance was permanent, clear and of significant value. It’s a reasonable strategy for a very tough market.
Nonetheless, we made considerable but isolated progress during the Obama Administration. Incentive programs by the Department of Health and Human Services (DHHS), particularly through the Substance Abuse and Mental Health Services Administration (SAMHSA), the Department of Housing and Urban Development (HUD), the Department of Justice (DoJ) and even the Department of Labor (DoL) all offered programs that promoted innovation towards a technology-enabled continuum of care. Our own work in substance use disorder, offender reentry and chronic physical health management saw tremendous results and recognition. (See this video by one of our clients.) However, without a compelling mandate with appropriate funding, there was no hope of fully developing these isolated successes into the ubiquitous solutions that can transform care.
Friends and critics alike asked “but what happens if a Republican administration takes office? Won’t you lose your value proposition as the country takes a more conservative approach to healthcare?” We were confident, OK, a bit arrogant. “Of course not. Our approach and solutions are so central to improving health outcomes and lowering cost that they are immune to political whims. In the end, the practicality of our solutions will win the day.”
We still think we are right, but we completely missed how impactful would be the period of uncertainty following the 2016 election, while the Republicans tried to repeal Obamacare. The uncertainty alone stifled innovation.
Reading the tea leaves.
We’re still looking for that one irrefutable policy or regulation that requires all providers to leverage telehealth technologies across the continuum of care. But in the meantime, the evidence is becoming clear that even if such a prominent mandate is not at hand, the sum of various policies and regulations is now sufficient to light the path towards transformation. Here are a summary of some of the most important policies, along with links to other posts or papers that explore them more fully:
The Support Act of 2018. The Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (“SUPPORT Act”), is a grab-bag of 120 separate bills designed to address the opioid crisis. Along with increasing capacity for addiction treatment, the SUPPORT Act includes incentives for programs such as housing, employment and offender reentry that are often associated with addiction. The SUPPORT Act does not contain an overarching requirement for technology enabled solutions, but several Sections that address specific programs include references to technology-enabled patient engagement and care collaboration. Read more.
2019 HUD Funding Guidance for Housing Programs. The 2019 Notice of Funding Availability (NOFA) [for the CoC program] allows communities “flexibility to impose service participation requirements for participants after they have been stabilized in housing. This reform will allow for greater local flexibility and innovation to drive successful outcomes for vulnerable homeless individuals.” Again, while this provision funding guidance does not expressly mention telehealth, this shift to allow housing providers to require participation in supporting services, like treatment for addiction, mental health or chronic medical conditions, as well as social care such as offender reentry or employment, directly addresses the policy of breaking down the silos while indirectly requiring the development of new telehealth technologies that bridge the gaps between the silos. Read more.
Executive Order on Protecting and Improving Medicare for Our Nation’s Seniors. On October 3, 2019, President Trump signed this Executive Order which, on the face of it, focuses on measures to promote Medicare Advantage programs and bring traditional Medicare more in line with the Administration’s view of market driven health insurance. However, just below the surface, are a series of provisions intended to promote telehealth innovation including new funding models. “Within 1 year of the date of this order, the Secretary [of DHHS] shall propose a regulation and implement other administrative actions to… encourage innovative MA benefit structures and plan designs, including through changes in regulations and guidance that… promote innovations in… telehealth services.” See the Executive Order here.
Through these policies alone, we see a focus on Medicaid, Medicare and permanent supportive housing providers to promote telehealth in support of an integrated continuum of care.
Do these policies constitute a trend?
In April, Manatt Health, for the Robert Wood Johnson Foundation published a report titled “Addressing Social Factors That Affect Health: Emerging Trends and Leading Edge Practices in Medicaid” that observed “States are entering a new phase of work related to SDOH: Moving beyond simply referring people to social supports and looking to ensure that people receive the services they need; as well as engaging Medicaid managed care companies more fully as partners in addressing social factors. Increasingly, SDOH interventions will be more closely integrated to the delivery of care.” (Manatt Health for Robert Woods Johnson Foundation, 4/19) Certainly this trend is in line with the above federal policies.
More recently, in September, the National Academies of Sciences, Engineering and Medicine published a report titled “Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health (2019).” Among the many important observations about the importance of an integrated continuum of care that includes social determinants is this: “The shift in the health care sector towards value based payments that incentivize prevention and improved health and health care outcomes for persons and populations rather than service delivery alone has made possible expanded approaches to addressing health-related factors that may be upstream from the clinical encounter.”
Thus, it is safe to conclude that the specific policies mentioned here are part of a larger trend at both the state and the federal level to move towards value-based care, which has at its core the creation of a technology-enabled integrated continuum of care.
But are these policies and trends enough?
Nonetheless, given the past history, we must ask, Is this trend and these policy initiatives enough to create a compelling case for telehealth innovation today? The answer is a definite Maybe. They certainly communicate that innovations in telehealth are recognized and supported by both major political parties, so the old question of would a Republican administration abandon a focus on telehealth has been answered. It will not. Further, while the fight over total funding for healthcare, and the battle between Medicare for All and market-based approaches are far from over, these policies show that whichever party wins the 2020 election and whichever overall health policy prevails, telehealth and the migration toward a truly integrated continuum of care are here to stay. If payers, particularly the MCOs and MAs can see the financial and competitive reward in today’s policies, it’s a reasonable bet that future policies will be even better.
Leadership is the key.
As with past policy initiatives, understanding the Administration’s intent is only half the puzzle. The other half is how payers react to the policies. MCOs and MAs are at the heart of this. If MCOs and MAs believe that these policies create an environment where promoting and rewarding telehealth solutions is in their individual best interest, not only to improve health outcomes and lower cost, but also to improve their profitability and competitive position, then we will see a well-funded push starting now.
Today might be too soon, but tomorrow will definitely be too late.
As we noted at the top, it is understandable that payers and providers may delay implementing new telehealth solutions until the mandate is absolutely clear and unavoidable. On the other hand, looking specifically at the MCOs and MAs, we think now is the time to invest in telehealth solutions that improve the experience of care for all stakeholders and contribute to an integrated continuum of care. Health and social care providers face the same choice, albeit constrained by the practice guidance and incentives they receive from MCOs, MAs and other payers. Ultimately, those organizations that are quick to recognize that this is a point of inflection for telehealth innovation and act on it will be in the best position for leadership and profitability for years to come.
Next steps.
We’ve been waiting for this moment for more than 10 years, so we know what to do to take advantage of this moment and contribute to this critical transformation. In our next post we will announce the proVizor Telehealth Community Project, to bring together leaders in health and social care, technology and research to develop the latest understanding of telehealth business requirements, functional requirements and technology solutions to improve outcomes and lower cost.
Conclusion.
Whatever happens in the 2020 election, the evidence is clear today that innovations in telehealth across the continuum of care will be at the fore. The time for telehealth solutions across the full continuum of care is at hand. Now is the time to get started.
Then again, we’ve been here before. Unless we see true leadership from payers and providers, this may be another wasted opportunity. Thus, now is the time for telehealth–maybe.

