Serious Mental Illness Care Unit Background Analysis
This is a working document. It is designed to foster discussion and advance ideas. It is not a final product and may not be used as such.
Introduction
In the United States, one in five people suffer from mental illness. That is about 57.7 million people every year. Up to two thirds of homeless adults suffer from chronic alcoholism, drug addiction, mental illness or some combination of the three. One fourth of all social security disability payments are for people with mental illness and almost half of Medicaid beneficiaries who have disabilities have a mental illness.
The evidence shows that people with mental health and addiction disorders also have higher rates of comorbidities including diabetes, COPD, hypertension and cancer not to mention HIV/AIDS and hepatitis C. According to the Substance Abuse & Mental Health Services Administration (SAMHSA), people with serious mental illness die 25 years sooner than the general population.
Note 1 Behavioral Healthcare, january/february 2013 volume 33 number 1
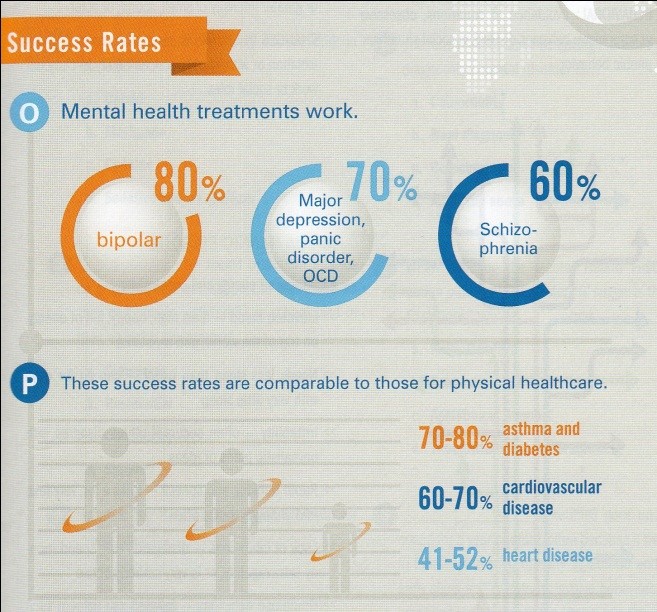
Mental and addiction health treatment works. Treatment of bipolar disorder, major depression, panic disorder, OCD and schizophrenia have been shown to improve health at rates that compare favorably to treatment of asthma & diabetes, cardiovascular disease and heart disease, yet fewer than one third of people with mental illness receive treatment, mostly as a result of limited access to care and stigma.
Racial and ethnic minorities are less likely to have access to mental health services and often receive poorer quality of care. The nation’s community behavioral health organizations employ about 250,000 people who care for 8 million adults and children with mental and addiction disorders. Between 2002 and 2011, the percentage of adults using outpatient mental health services in the past year declined from 7.4 to 6.7 percent, and the percentage using prescription medication for a mental health problem increased from 10.5 to 11.5 percent.
Mental illness constitutes about 6.2% of the nation’s spending on healthcare, but unlike other medical disorders, the costs of mental disorders are more “indirect” than “direct” (Insel, 2008).
Direct costs include the costs of care (e.g. medications, clinic visits, hospitalization) while indirect costs are incurred through reduced labor supply, public income support payments, reduced educational attainment and costs of other consequences like incarceration and homelessness. One recent study estimates that serious mental illnesses cost society $255.4 billion annually in lost earnings.
The purpose of this analysis is to consider if and how technology-enabled Patient Relationship Management can improve outcomes and lower cost with respect to patients in community-based mental and addiction health programs. This will be referred to as the “Mental Health Care Unit.”
This analysis is intended to express a general set of requirements and approach to the Mental Health Care Unit. The method for analysis follows a model (The Care Unit Method) developed by White Pine Systems which has been used for several years by teams of graduate students from Indiana University-Purdue University at Indianapolis (IUPUI) and applied to various health interests including diabetes, juvenile obesity and hypertension.

